

Leveraging SOGI and REAL Data to Advance Equity in Behavioral Health: Key Learnings
By Naomi Miller-Altuner
On February 22nd, 2023, over 250 people attended the webinar: Leveraging SOGI and REAL Data to Advance Equity in Behavioral Health. Hosted by the California Institute for Behavioral Health Solutions (CIBHS) and co-sponsored by the California Primary Care Association (CPCA) and the County Behavioral Health Directors Association of California (CBHDA) in partnership with JSI, the webinar came to fruition as a part of Delta Center California. Peter Dy of CPCA and Elissa Feld of CBHDA moderated the webinar panel which featured five speakers:
-
Dr. Alex Keuroghlian, MD, MPH, Director, Division of Equity & Training at The Fenway Institute
- Dr. David Tian, MD, MPP, FASAM, Medical Consultant II, DHCS
- Dr. Vanessa Blum, PhD, Clinical Psychologist, Marin County Behavioral Health & Recovery Services
- Gabriel Garcia-Lopez, Director of Health Information Systems, Los Angeles LGBT Center
- Tracy Lacey, LMFT, Senior Mental Health Services Manager, Solano County Behavioral Health
During the webinar, panelists explained the critical importance of Sexual Orientation and Gender Identity (SOGI) and Race, Ethnicity, and Language (REAL) data collection in providing inclusive, quality care.
Historical inequities and discrimination perpetuated by healthcare systems and bias among healthcare professionals has led to widespread mistrust of healthcare institutions among communities of color and LGBTQIA+ communities. Too often, these groups experience discrimination, stigma, and subsequent poor health outcomes. SOGI and REAL data enable providers to identify and better understand these inequities, tailoring care to meet the specific needs of their clients; to practice gender affirming and culturally humble care; and ultimately to ensure health systems are truly in service of LGBTQIA+ and BIPOC communities.
The panelists provided context on the current state of SOGI and REAL data collection in California and nationally and offered recommendations for providers and clinics preparing to collect this data. They also discussed the impact of state and federal policies and regulations on the collection of SOGI and REAL data in clinical settings. Their presentations were rich with information, recommendations, and resources. This summary highlights key themes discussed and resources shared by panelists. The webinar recording is available here and the slides are available here.
Collecting SOGI Data in a Systematic and Sensitive Manner
Clinical Implications of SOGI Data
Dr. Keuroghlian shared a story about a deidentified patient named Rodrigo, a 40-year-old trans man who did not feel comfortable disclosing his trans status to his healthcare provider. One day, Rodrigo came into the clinic with pelvic pain and vaginal spotting. It turned out that Rodrigo had cervical cancer, which could have been prevented with a routine cervical pap test. None of his providers had thought to perform this preventative test, in part because no one had asked Rodrigo about his sex assigned at birth.
Unfortunately it is common for providers to refrain from asking these questions as they assume patients will feel offended if asked to discuss their SOGI. Dr. Keuroghlian noted that in reality “the rudest thing we can do and the way we're going to offend people is by not asking for this critical health-related information and having these really unfortunate adverse health outcomes for patients that are preventable.” In fact, according to studies performed by the Fenway Institute and others, the overwhelming majority of patients across the nation, including cis-gendered straight people, are actually happy to answer questions about their SOGI. Dr. Keuroghlian says SOGI data must be collected in a “systematic and sensitive” way, as part of the standard process for registering and intaking patients. The opportunity to disclose health-related SOGI information must be integrated into the care model and not left up to individual patient-provider interactions.
Population Health Implications of SOGI and REAL Data
Gabriel Garcia-Lopez spoke about the importance of SOGI and REAL data collection from a community health center perspective. The LA LGBT Center, an FQHC, is the nation’s largest provider of LGBT medical and mental health services. The center collects SOGI data via their customized electronic health record. From a population health standpoint, this provides useful information for identifying communities that may be experiencing greater risk for certain adverse health outcomes.
According to Mr. Garcia-Lopez, “because these fields exist as discrete and structured data within the EMR, we're able to pull that for analytics purposes.” This data is in turn helpful for identifying and responding to community-wide trends in health outcomes. Similarly, Tracy Lacey shared that in Solano County, the inclusion of SOGI and REAL data in their electronic health record has allowed school-based mobile crisis call centers to disaggregate their data by sexual orientation, gender identity, and race. This information helps to highlight where behavioral health services are most needed. For example, through analyzing call center data, Solano County has identified that LGBTQIA+ students are at particularly high risk for suicide. In turn, this data fostered a call to action for local school districts to implement suicide awareness trainings for students and staff.
Ending the Invisibility of LGBTQIA+ People in Healthcare: The Importance of Inclusive Language
Dr. Vanessa Blum, a Clinical Psychologist with Marin County Behavioral Health & Recovery Services (BHRS), spoke to the importance of using inclusive language in clinical care settings and data collection. Marin County BHRS recently updated their client profile form to be trauma-informed and to reflect more inclusive language. The updated form asks clients to indicate their chosen name, pronouns, and sex assigned at birth. It also reflects updated sexual orientation terminology, including a write-in option and a “decline to state” option. Many webinar attendees reflected that the terminology of “chosen name” is a wonderful way to help someone feel accepted. Dr. Blum and her colleagues also implemented what they call a “roadshow” approach to training their staff on the new form. This means they bring the training session to each team within BHRS, ensure all staff receive the training, and increase staff engagement and participation.
Throughout the webinar, speakers offered other helpful recommendations for using inclusive language and for making a clinical space more inclusive for all:
- If you make a mistake (i.e., refer to a patient using the incorrect pronoun), the best thing to do is to apologize, correct yourself, and then move on.
- Avoid assumptions. If you do not know a patient or client’s pronouns, use language that does not assume a gender.
- If you are unsure of a patient’s preferred name or pronouns, it is okay to ask.
- Create a work environment of accountability and respect. It is appropriate and important to politely correct a colleague if they use incorrect or inappropriate language.
- Use gender-inclusive diagrams and images in patient education materials.
- Offer patient education materials in a variety of languages.
- Make the physical clinic a more inclusive space (i.e., posters and artwork that represent communities served, gender inclusive bathroom signs, pronoun pins for staff).
These changes around language and physical environment signal to patients and clients that they are welcome and accepted, regardless of their sexual orientation, gender identity, race, ethnicity, or language(s) spoken. As Tracy Lacey put it, these changes “help the invisible to be seen.”
SOGI Data Collection in Pediatric Patient Populations
Throughout this webinar, multiple panelists highlighted the importance of collecting SOGI data within pediatric populations. According to Dr. Keuroghlian, from 3 years of age, patients are able to communicate their gender identity. The Fenway Institute recommends that providers begin discussing gender identity well before puberty and that they begin discussing sexual orientation at the same time they discuss puberty, which is typically at about 12 years of age. Whenever possible, these questions should be asked in private.
Similarly, Tracy Lacey shared the approach Solano County Behavioral Health has developed in partnership with UC Davis, local community-based organizations, and community members. Through this collaborative project, Solano County convened a workgroup to develop culturally responsive self-reporting tools for their clients. Ms. Lacey spoke to Solano County’s conscious decision to begin collecting SOGI data starting at age 10. This decision was influenced, in part, by the prevalence of commercial sexual exploitation within the county, with the average age of victims being 10 years old. Ms. Lacey also emphasized unique considerations for collecting SOGI data among youth. For example, it is important to consider that some youth may be hesitant or unwilling to share SOGI related information in front of their parents. Thus, Solano County Behavioral Health created a self reporting tool for parents and a separate tool for youth to fill out in a room with only the provider present. This better supports youth in sharing SOGI related information with their provider. Importantly, in an effort to collect SOGI data in a responsive and effective way, the county has sought opportunities for youth and members of the LGBTQIA+ community to provide feedback on how this information is being collected.
State and Federal Regulations on SOGI and REAL Data Collection Practices
Dr. David Tian presented the current state of SOGI and REAL data collection practices in the State of California. Dr. Tian noted that many factors – intersecting federal and state laws, guidance from the Center for Medicare and Medicaid Services, data mapping standards, among other considerations – guide and, at times, constrain what data DHCS can collect. For example, due to federal restrictions, the paper form of the Medi-Cal application only has options for an applicant to select “male” or “female.” DHCS has more flexibility in the questions they ask on the online Medi-Cal application. This version of the form includes additional options for a patient to communicate their gender identity. Dr. Tian noted that DHCS also receives data from other public programs, giving DHCS access to richer sets of SOGI data. Finally, DHCS has incentivized the collection of SOGI data in public hospitals in California, encouraging hospitals to “increasingly collect complete data, in better and better ways over succeeding years.”
Dr. Tian also discussed DHCS’ current REAL data collection practices, which are similarly influenced by both state and federal policies and regulations. Dr. Tian emphasized that many people, particularly BIPOC individuals, often feel uncomfortable sharing REAL information, especially given historical and current discrimination against communities of color. This has resulted in a high “no response” rate for REAL data collection. Thus, REAL data may be inaccurate or simply unavailable. According to Dr. Tian, the availability of SOGI and REAL data is “incumbent on all public agencies to build trust with communities and people in our community, so that they are comfortable sharing this information.” The collection of SOGI and REAL data depends upon, and can help establish, trusting and safe relationships between healthcare systems and BIPOC and LGBTQIA+ communities.
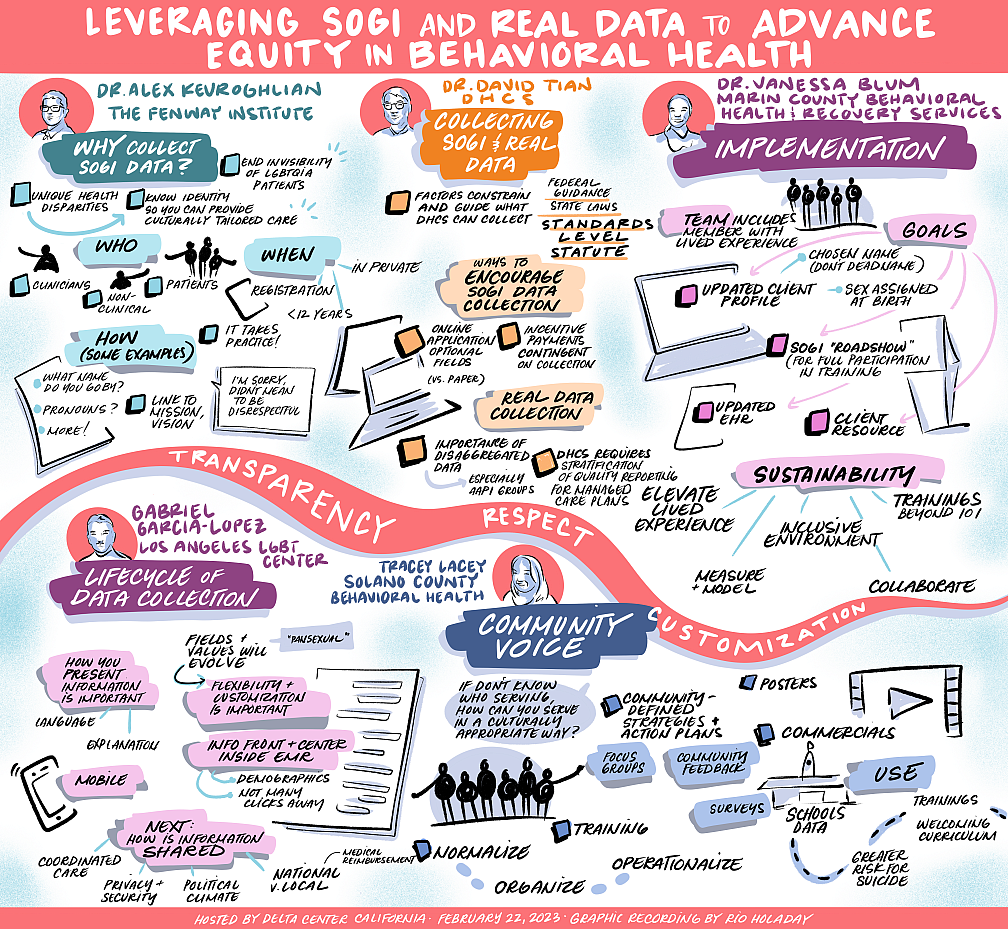
Graphic recording by Rio Holaday
Resources
- The National LGBTQIA+ Health Education Center - A Program of the Fenway Institute: Many resources, publications, learning modules and webinars
- Ready, Set, Go! Guidelines and Tips For Collecting Patient Data on Sexual Orientation and Gender Identity (SOGI) – 2022 Update (National LGBTQIA+ Health Education Center - A Program of the Fenway Institute)
- SO/GI Data Collection Demonstration Videos (The National LGBTQIA+ Health Education Center - A Program of the Fenway Institute)
- Learning Resources — Collecting Sexual Orientation and Gender Identity Data (The National LGBTQIA+ Health Education Center - A Program of the Fenway Institute)
- Focus on Forms and Policy: Creating an Inclusive Environment for LGBT Patients (The National LGBTQIA+ Health Education Center - A Program of the Fenway Institute)
- Learning to Address Implicit Bias Towards LGBTQ Patients: Case Scenarios (The National LGBTQIA+ Health Education Center - A Program of the Fenway Institute)
- Solano County Behavioral Health: Media Campaigns (Solano County Behavioral Health)